Irrational Use of Medicine in Bangladesh: Graduate Pharmacists Are the Key
The interim government's initiative to launch chain pharmacies and the plan to distribute essential medicines through graduate pharmacists in hospitals could be a groundbreaking step in healthcare

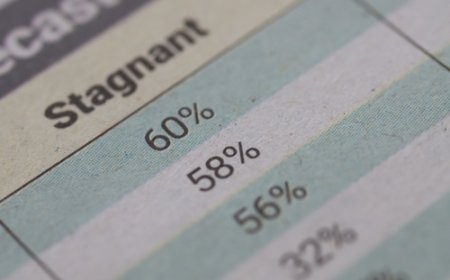
It is estimated that more than half of all medicines worldwide are prescribed, dispensed, or sold inappropriately -- and that half of all patients do not take their medicines correctly.
This leads to a massive waste of valuable resources and significantly increases health risks. The problem is particularly severe in low- and middle-income countries, especially in Africa and South Asia.
Now, let’s take a closer look at the situation in Bangladesh, where drug use is largely unregulated. The country’s healthcare system generally follows two main pathways: government hospitals and private clinics or hospitals.
Since the private system is largely profit-driven, we tend to consider government hospitals as the ideal standard. A typical patient visiting a public hospital goes to the pharmacy for medicines after consultations and diagnostic tests, and since most essential medicines are not readily available in public hospitals, patients are often forced to buy them from outside.
But regardless of whether the medicine is sourced from the hospital pharmacy or a local drug store, it is very important that patients receive proper guidance on how to use their medicines effectively.
This is exactly where the WHO's concern about improper prescription and distribution becomes highly relevant. In this context, the question arises -- how can we ensure the rational use of medicine?
Bangladesh is currently experiencing a wave of constructive change across various sectors. So now is the perfect time to take effective steps to ensure proper medicine management.
At the centre of this initiative can be the graduate pharmacist. They will ensure that the right medicine is provided, in the right dose, for the right duration, tailored to the specific patient, and at the lowest possible cost. As a result, not only will recovery rates improve, but public trust in the healthcare system will also grow.
This is why the interim government's initiative to launch chain pharmacies and the plan to distribute essential medicines through graduate pharmacists in hospitals could be a groundbreaking step in healthcare.
According to the World Health Organization (WHO), three of the main causes of irrational medicine use are prescription errors, transcription errors, and dispensing errors. Qualified and trained pharmacists can be the key solution in these areas.
Firstly, doctors in our country often face an overwhelming number of patients -- sometimes to an inhumane extent. This excessive pressure can lead to prescription errors and irrational medicine use. In such cases, pharmacists can act as a support system to reduce that burden. They can provide patients with accurate guidance on how to use medicines, explain side effects, and offer necessary counseling. As a result, proper medicine use will reduce the number of illnesses and patients, easing the pressure on doctors and lowering healthcare costs.
Secondly, when pharmacists are responsible for dispensing medicines, the rate of dispensing and transcription related irrational use can also be reduced.
At the same time, when graduate pharmacists ensure proper storage, maintenance, and supply of medicines based on demand, it becomes easier to maintain quality standards. This will reduce the risk of stock-outs and help prevent the unauthorized sale and distribution of medicines without prescriptions.
Many private hospitals have already begun incorporating hospital pharmacy practice, and even clinical pharmacy is gaining ground. Once public hospitals fully adopt this model, the private sector will likely follow, broadening access to quality healthcare.
In this new reality, it is extremely important that the generic names of medicines are prescribed. Since the exact brands available in pharmacies can vary, using a generic name ensures flexibility and avoids brand bias. The government typically procures medicines through a competitive bidding process that prioritizes both quality and affordability. Insisting on a specific brand may not only create bias but also make procurement and supply more difficult.
Previously, the main reason for prescribing by brand name was the lack of qualified pharmacists at pharmacies. Doctors felt uncertain about the quality of medicines being dispensed. Now, with graduate pharmacists in place, these concerns are largely resolved. Pharmacists are the most knowledgeable professionals when it comes to every stage of a medicine’s lifecycle -- from production to distribution. With them in charge, the public is bound to benefit.
Hospital pharmacy is not a new concept globally. In the United States, the first hospital pharmacy began in 1752 at Pennsylvania Hospital, where Jonathan Roberts was appointed as the first apothecary. The profession became more organized and standardized in the 1950s. In the UK, the first official hospital pharmacist was appointed in 1844 at Guy’s Hospital in London. Across Europe, hospital pharmacy flourished after World War II, along with the expansion of national healthcare systems.
I firmly believe hospital pharmacies will be established in Bangladesh as well -- whether it happens now or a decade later. However, this shouldn’t be done merely to follow the developed world.
For a developing country like ours, hospital pharmacy is essential if we are to reduce healthcare costs and ensure quality services. If we fail to start this vital reform today, the consequences will inevitably be borne by our future generations.
Mahady Tarek is a pharmacist working with an international humanitarian organization.
What's Your Reaction?